1-Minute Summary
- The FDA's "Big List" includes nine major allergens, highlighting the need for accurate labeling and allergen controls in food manufacturing.
- Effective allergen controls and preventive measures are essential under the Food Safety Modernization Act.
- Rigorous supplier audits and emergency management are critical when switching suppliers to prevent allergen introduction.
- Laboratory testing methods, including Lateral Flow, ELISA, and PCR, are key for identifying allergens in food manufacturing.
- Adherence to Hazard Analysis and Risk-Based Preventative Controls is mandatory for both domestic and foreign food facilities.
The Food Safety Modernization Act (FSMA), 21 CFR Part 117, significantly shifted the focus to “allergen cross-contact” from its earlier food-safety iteration of Good Manufacturing Practices (GMPs) found in 21 CFR Part 110.
The term “allergen cross-contact” was not even mentioned in Part 110, but it appears 37 times in Part 117, indicating the priority U.S. FDA places on prevention.
With sesame the latest addition to the FDA’s “Big List” of food allergens, and undeclared allergens the top reason for food recalls in 2023, it’s clear that developing allergen controls and avoiding allergen cross-contact are more important than ever for food manufacturers.
In this article, we provide key points to consider when developing your preventive allergen controls.
What is Allergen Cross-Contact?
Allergen cross-contact occurs when a non-allergenic food comes into contact with an allergenic food, leading to the unintentional transfer of allergens.
This can happen during various stages of food processing and handling, including production, packaging, and storage.
- Allergen cross-contact often occurs through shared equipment or utensils.
- Preventing allergen cross-contact is crucial in manufacturing environments that handle both allergenic and non-allergenic foods.

How is Allergen Cross-Contact Different than Cross-Contamination?
Though the terms are often used interchangeably, there are differences.
Allergen cross-contamination is a sub-category of cross-contact. It refers to the contamination of food products with allergenic food due to poor hygiene practices or improper handling.
In the case of allergen cross-contact, picture a food handler using a container that contained wheat to store a different product without sanitizing it first. The handler may inadvertently transfer a small amount of wheat to the other product, triggering an adverse reaction.
In the case of allergen cross-contamination, picture a food handler cutting meat and then switching to another ingredient without washing the knife. Cross-contamination can occur due to poor handling.
What Food Allergens are of Greatest Concern?
Most food allergies are caused by one or more allergenic proteins. FDA includes nine major food allergens in its “Big List”:
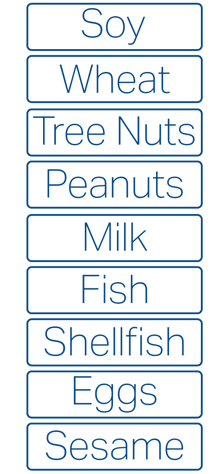
The presence of any of these nine allergens must be declared on a product’s label in accordance with the Food Allergen Labeling and Consumer Protection Act (FALCPA).
Both the U.S. food and dietary supplement industries are subject to FALCPA, which requires the allergen to be listed using its common name, making preventive allergen controls a necessary part of your process.
A note of exemption: Highly refined oils are exempt if processing removes all traces of the allergen.
Allergens in Food are Often Unintentional
Undeclared allergens continue to be responsible for the highest percentage of reported food recalls. They enter the food supply through…
- Breakdowns in processing, labeling, and storage.
- Communication gaps between suppliers, co-packers, and manufacturers.
Implementing effective allergen controls can address these inadvertent errors.
Intentional Allergen Contamination Can Qualify as Food Fraud
In other instances, allergens are knowingly included in the product, but their declaration on the label is intentionally and illegally avoided.
If this intentional adulteration is for economic gain, then the practice is known as “food fraud”.
However, if the adulteration is with the intent to cause harm, then it falls under the category of “food defense”.
In FDA’s eyes, the inclusion of an undeclared allergen in food or dietary supplements is an egregious error and can be punished through one or more FDA enforcement actions.

U.S. FDA Tips for Preventing Allergen Cross-Contact During Manufacturing
The U.S. FDA has published a helpful document entitled “Allergen Cross-Contact Prevention” that contains tips for developing preventive allergen controls that guard against allergen cross-contact in food manufacturing facilities. Here are the highlights, but consult the document for details:
- Implement Processing Controls: Include procedures like process scheduling, traffic control, physical segregation, and air filtration to prevent allergen cross-contact.
- Education and Training: Ensure staff are trained in identifying allergens, principles of cross-contact prevention, and specific protocols for prevention, including corrective actions.
- Receiving and Storage Controls: Verify labels and ingredients upon receipt, handle damaged packages carefully, and use clear identification for allergen content. Implement segregation and distinct markings for allergen-containing materials.
- Processing Considerations: Design facilities and equipment to minimize allergen cross-contact, use dedicated tools and apparel, and control material movement and airflow.
- Production Scheduling: Schedule production runs to separate allergen-containing and non-allergen products and consider clustering allergen-containing runs.
- Handling Rework and WIP: Store rework and work-in-progress (WIP) in labeled containers, establish tracking systems, and ensure allergen information is attached to each container.
Managing Allergen Risks When Switching Suppliers
Switching suppliers is a major factor in potential allergen cross-contact in food manufacturing, as the Covid-19 pandemic showed. Supply chain problems are still plaguing many manufacturers, which increases risk, especially when different suppliers have varying allergen control practices.
Here's how to mitigate this risk:
Rigorous Supplier Audits
- Conduct thorough assessments of new suppliers' allergen control procedures.
- Include both internal and third-party audits.
- Perform laboratory testing of supplied ingredients.
- Evaluate detailed ingredient specifications.
Effective Cleaning and Equipment Management
- As always, ensure meticulous cleaning of utensils and equipment to prevent allergen cross-contact.
Emergency Management for Unavoidable Supplier Changes
- Cease production using suspect ingredients immediately.
- Set aside unused ingredients for thorough evaluation.
- Implement traceability of the supply chain both backward and forward.

How Allergens are Identified in Laboratory Testing
Laboratory testing for allergens plays a crucial role in identifying allergens, either within the processing facility or through an independent third-party lab. Key methods include:
- Lateral Flow: Commonly used in manufacturing facilities, this method detects the presence or absence of allergens.
- ELISA (Enzyme-Linked Immunosorbent Assay): Provides quantitative assessment of allergens.
- PCR (Polymerase Chain Reaction): Targets DNA molecules post-thermal processing, but it's limited as it cannot distinguish specific DNA types.
- ATP Swabbing: Often used as an alternative to Lateral Flow and ELISA, but it may lack sensitivity as it detects only general proteins.
These testing methods help quantify and confirm the presence of allergens, ensuring food safety compliance.
Allergen Changeover Testing
Allergen changeover testing, when more than one product is produced on the same production line, is used to validate efficiency of sanitation. Cleaning is not enough to prevent allergen cross-contact; sanitizing and confirmation testing must follow.
Test products made in the first run after cleaning and sanitizing is complete to assess changeover effectiveness.
If positive results are found, corrective actions, including recleaning and sanitizing, must be undertaken, and that first-run product should be held or destroyed.
A single test may give an incomplete picture; therefore, a risk-based approach includes routine and random testing of equipment surfaces and food in appropriate intervals by zone, such as with an environmental monitoring program.
Allergen Controls are a Must for Processors & Suppliers
FSMA requires that both domestic and foreign food facilities conduct a hazard analysis for foreseeable food-safety risks, including the introduction of allergens, and to implement a system of risk-based preventive controls for those identified hazards.
Known as Hazard Analysis and Risk-Based Preventative Controls, an allergen control program is included as part of this hazard assessment and preventive strategy.
Allergen control programs are a must for both domestic food processors and their suppliers, including importers of food products. Steven Gendel, former FDA Food Allergen Coordinator, provides tips for designing your allergen control program here.
Integral to the overall preventive control-based food-safety program, monitoring for introduction of allergens, developing and implementing corrective-action procedures as necessary, and allergen testing are three major components.
Laboratory Accreditation and Certification
Food safety testing laboratories must have the equipment, methods, and expertise to ensure accurate identification of allergens. ISO 17025 accreditation demonstrates competency and provides assurance of accurate, traceable, and reproducible data based.
If you need allergen testing, Certified Laboratories can help.
Our regulatory partners at EAS Consulting Group, a Certified Group Company, can help you develop and assess your Hazard Analysis and Preventive Controls as well as your allergen control program at the supplier and manufacturer level.
For more on food allergen controls, check out our free webinar: Food Allergens and the FDA